What Herbs Help After a Hysterectomy
Table of Contents
Sometimes, surgery just needs to happen. Here’s how your hormone levels are affected, and what you can do to restore balance.
What is a hysterectomy?
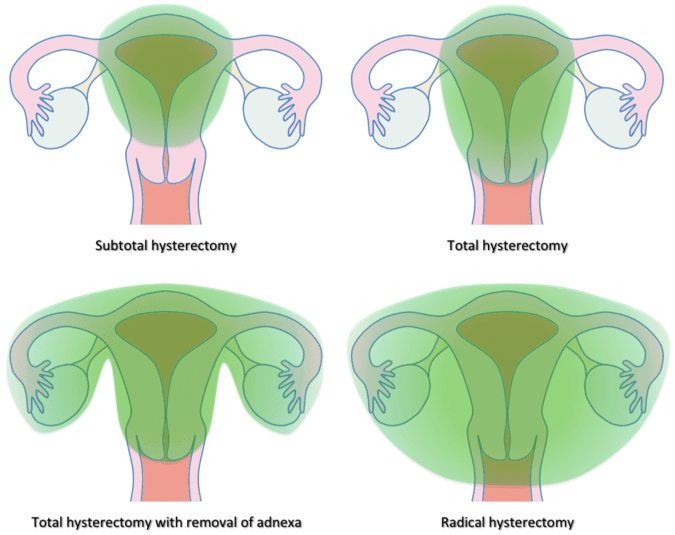
A hysterectomy is the surgical removal of a woman’s uterus, and when it’s just the uterus being removed – no other organs, except perhaps the cervix and surrounding, supporting tissues – it’s often referred to as a “partial hysterectomy.” But the procedure can also necessitate the removal of the ovaries as well, and technically, the name for that – ovary removal – is an “oophorectomy.” While your uterus does not produce hormones, your ovaries do – and that’s what we want to talk about here: how your hormones are affected by either procedure.
Now, the decision to remove a uterus is deeply personal and can be scary for some. But often – as is the case with uterine fibroids, endometriosis, or uterine prolapse – the surgery is unavoidable. Most women aren’t told however what will happen to them after a hysterectomy, and as a result, many suffer for years because of one symptom or another, either directly from the loss of proper estrogen and progesterone production, or indirectly from the cascading impact on other hormones.
If a hysterectomy is in your future, or if you’ve had one already, you can expect to experience some hormone changes. But fortunately, there are powerful tools out there to navigate those changes, and start feeling like yourself again. Let’s look at some of the reasons you (or your doctor) might be considering a hysterectomy, how it (or it in conjunction with oophorectomy) affects hormone production, and steps to take afterward to reestablish balance.
Reasons for Getting A Hysterectomy

According to the National Women’s Health Information Center, one in three women in the United States has had a hysterectomy by age 60. This is due to a variety of reasons, including improving quality of life, correct a serious problem that is interfering with a woman’s normal bodily function, or in more severe cases, to save one’s life. But demographically, the numbers are shifting. As Women in Balance Institute notes,
Centers for Disease Control statistics show that the number of hysterectomies is actually starting to decline, especially in the 50-54 age group, and hysterectomy rates are higher in the South of the country and lowest in the Northeast, where rates continue to decline significantly.
The article also points out that many hysterectomies may be unnecessary since alternatives for conditions like heavy periods or chronic pelvic pain are on the rise. As a result, a hysterectomy is starting to seem like a last resort.
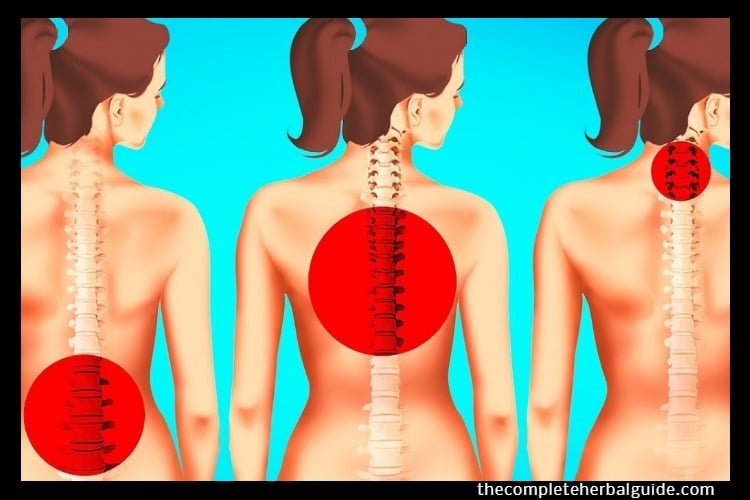
Identifying Hormone Imbalance Early On
Still: the fact remains that sometimes, a hysterectomy is critical. Cancer of the uterus, ovaries, or cervix usually necessitates this procedure. But most hysterectomies are performed for non-cancerous conditions, such as uterine fibroids, which cause pain and bleeding, or uterine prolapse: a sliding of the uterus from its normal position into the vaginal canal. The bottom line here is advocating for yourself: when discussing treatment options for your condition with your doctor, just know that a hysterectomy isn’t always necessary if you don’t want it.
How Hysterectomy Affects Hormone Production
As we mentioned earlier, a “pure” hysterectomy involves the removal of your uterus, an organ that does not produce hormones – your ovaries do. So, with your uterus removed, hormone imbalance shouldn’t even be a thing, right? Not so fast. As OB-GYN Marcelle Pick of Women to Women writes,
“Reports show than more than half of all women who undergo hysterectomy but retain their ovaries will experience symptoms of hormone shifting and imbalance – even though their ovaries are left in place and continue to function. What many women aren’t told is that the uterus and ovaries share their blood supply and once the uterus is removed, ovarian function can be negatively affected.”
So even if your hysterectomy just affects your uterus, you can most likely expect hormone changes.
However, in the case of a hysterectomy and oophorectomy – the removal of your ovaries – you can definitely expect hormone change because your ovaries produce estrogen and progesterone. Again, from the Women in Balance Institute:
“Removal of the ovaries (“oophorectomy”) induces “surgical menopause,” suddenly placing a woman in a state of ovarian hormone deficiency that would normally have occurred over several years during a natural menopausal transition. Ovarian hormones, primarily estrogens, and progesterone play an important role in protecting the health of organs such as the heart, bones, brain, and breasts.”
So in short: when this procedure involves ovary removal, early menopause is a given. You may remember Angelina Jolie writing about this experience a few years ago when she made the decision to have these organs removed, in order to ward off the risk of ovarian cancer (which runs in her family).
How to Get Your Hormones Back in Balance
Whether you’re trying to balance your hormones to lessen the chances you’ll need a hysterectomy (i.e., trying to prevent the growth of fibroids and endometriosis), or manage the hormonal aftermath post-surgery, there are specific steps you can take to get your estrogen and progesterone levels – and in turn, your overall hormone balance – back to a healthy place.
One route after hysterectomy is estrogen replacement therapy. And for many women, this is a perfectly viable option: ET (estrogen therapy) can help treat menopausal hot flashes and night sweats, and ease vaginal symptoms of menopause, such as dryness, itching, burning and discomfort with intercourse – and, it can do all this in the short-term.
But ET doesn’t come without significant drawbacks, such as a slight risk of stroke, blood clots, and gallstones. It also – when administered as part of a combined hormone therapy program – comes with an increased risk of breast cancer, as noted by the National Cancer Institute.
There is, however, another option for balancing your hormones: a supplementation program that encourages your body to make more of the hormones it needs. It’s more gradual than HRT (hormone replacement therapy), but it won’t inflate your hormones to artificially high levels, or put you at risk for the conditions sometimes associated with HRT.
What Herbs Help After a Hysterectomy?

“There are herbs like black cohosh, ashwagandha, red clover and chasteberry which are known to provide support for the sex hormones (estrogen, progesterone, and testosterone) which fluctuate after a hysterectomy,” says Pick. She also notes that many women will report having persistent hot flashes after hysterectomy, and for that, she recommends “soy isoflavones – about 80 mg a day. I suggest that you chose soy which is derived from the whole bean (not the germ) in either powder or pill form. I also recommend a high-quality multivitamin/mineral complex dietary supplement. It’s a great way to support your body and ensure that you are getting the nutrients you need during a time of hormonal transition.”
(Note: These are all supplements you can take before hysterectomy as well, to help ward off conditions that might lead to one.)
Chasteberry, in particular, encourages your body to produce more progesterone, your “youth” hormone that is particularly affected by menopause. When its levels are healthy, estrogen is kept in check as well – ensuring you don’t enter a state of estrogen dominance, and the hot flashes / sleepless nights that come with it.
Whether or not a hysterectomy is in your future, it’s important for all women to be armed with information about their hormonal health. Here’s to you!
LEARN MORE...