Natural Remedies for Macular Degeneration
Table of Contents
Symptoms Include:
- Visual distortions, such as straight lines appearing wavy or crooked
- Objects appearing smaller or farther away than they should
- A decline in or loss of central vision
- Central blurry spot
In either form of macular degeneration, your vision may falter in one eye while the other has no problem for years. You may not notice any or much change because your good eye compensates for the weak one. Your vision and lifestyle begin to be dramatically affected when this condition develops in both eyes.
Hallucinations
Some people with macular degeneration may experience visual hallucinations, as their vision loss gets worse.
These hallucinations may include:
- Unusual patterns
- Geometric figures
- Animals
- Grotesque-appearing faces
While these hallucinations may be frightening, they are not a sign of mental illness. These hallucinations are so common that there is a name for this occurrence called, “The Charles Bonnet syndrome.”
Causes
Researchers do not know the exact causes of macular degeneration, but they have identified some contributing factors, including:
- Age
- Family history of macular degeneration
- Race: Macular degeneration is more common in whites than it is in other groups, especially after age 75.
- Sex: Women are more likely than men are to develop macular degeneration.
- Cigarette smoking: Exposure to cigarette smoke doubles your risk of macular degeneration. Cigarette smoking is the most preventable cause of macular degeneration.
- Obesity
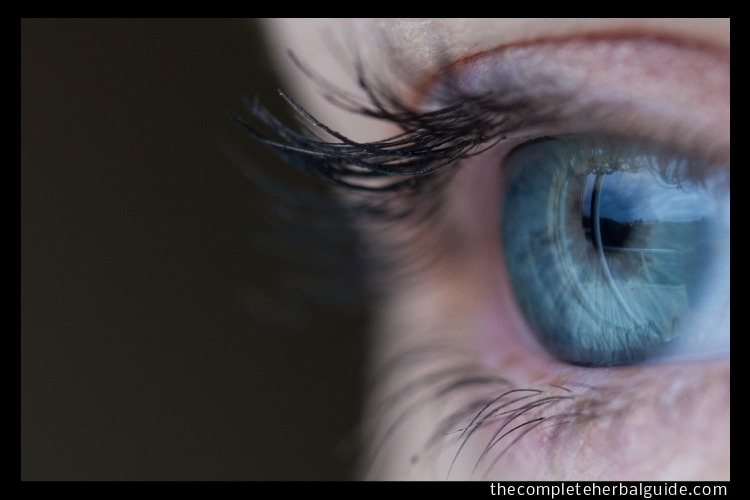
- Light-colored eyes: People with light-colored eyes appear to be at greater risk than do those with darker eyes.
- Exposure to sunlight: It is possible that long-term exposure to ultraviolet light may increase your risk of developing macular degeneration, but this risk has not been proved and remains controversial.
- Low levels of nutrients: This includes low blood levels of minerals, such as zinc, and of antioxidant vitamins, such as A, C and E. Antioxidants may protect your cells from oxygen damage (oxidation), which may partially be responsible for the effects of aging and for the development of certain diseases such as macular degeneration.
- Cardiovascular diseases: These include high blood pressure, stroke, heart attack and coronary artery disease with chest pain (angina).
Diagnosis
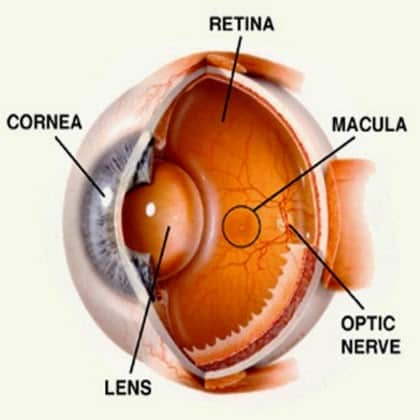
To determine whether you have macular degeneration, you will undergo a thorough eye examination. One of the things your eye doctor looks for while examining the inside of your eye is the presence of drusen and mottled pigmentation in the macula.
The eye examination includes a simple test of your central vision and may include testing with an Amsler grid. If you have macular degeneration, when you look at the grid some of the straight lines may seem faded, broken or distorted. By noting where the break or distortion occurs — usually on or near the center of the grid — your eye doctor can better determine the location and extent of your macular damage.
Other diagnostic tests may include
Angiography
To evaluate the extent of the damage from macular degeneration, your eye doctor may use fluorescein angiography. In this procedure, fluorescein dye is injected into a vein in your arm and photographs are taken off the back of the eye as the dye passes through blood vessels in your retina and choroid. Your doctor then uses these photographs to detect changes in macular pigmentation or the existence of abnormal blood vessels in your macula that may not be visible or recognizable during a standard examination.
Indocyanine green angiography
Instead of fluorescein, a dye called indocyanine green (ICG) is used. This test provides information that complements the findings obtained through fluorescein angiography.
Optical coherence tomography (OCT)
This noninvasive imaging test helps identify and display areas of retinal thickening or thinning. Such changes are associated with macular degeneration. This test can also reveal the presence of abnormal fluid in and under the retina or the RPE. It’s often used to help monitor the response of the retina to macular degeneration treatments.
Genetic screening
Even though genetic abnormalities have been identified in some people with macular degeneration, genetic screening tests are not currently being used to diagnose the disorder, though they may be used to assess early risk in the future.
Treatment
Some treatment options are available for wet macular degeneration. But the success of the treatment — stopping further progress of the disease — depends on the location and the extent of the abnormal blood vessels, or choroidal neovascularization (CNV). The damage already caused by macular degeneration cannot be reversed. The sooner CNV is detected, the better your chances of treatment preserving what’s left of your central vision.
Wet macular degeneration treatments are procedures for wet macular degeneration, all of which can be done on an outpatient basis, include:
Photocoagulation
In photocoagulation, your doctor uses a high-energy laser beam to create small burns in areas with abnormal blood vessels. The process can seal off and destroy the CNV that has developed under your macula. It can prevent further damage to the macula and halt continued vision loss.
Photodynamic therapy (PDT)
This therapy is primarily used for treating CNV that is located directly under the fovea. The fovea lies at the center of your macula and in healthy eyes provides your sharpest vision. If conventional hot-laser surgery were used at this location, it would destroy all central vision. PDT increases your chances of preserving some of that vision. It will not bring back any of the vision you have lost, but it may halt the loss of your vision or at least slow down the rate of vision loss.
Macular translocation surgery
Macular translocation surgery is a treatment that can be used if the abnormal blood vessels are located directly under the fovea. To start the procedure, your surgeon detaches the retina, shifts the fovea away from the CNV and relocates it over healthy tissue. When the CNV is exposed, the surgeon can remove the CNV with tiny forceps or use a hot laser to destroy blood vessels without damaging the fovea. This surgery can be successful for preserving vision, and in some instances improving vision, if your vision loss is recent, the extent of CNV is limited and the tissue around the fovea is healthy. This surgery is not widely used.
The newest treatment being used for macular degeneration involves use of drugs called anti-vascular endothelial growth factor (anti-VEGF) medications. These drugs help stop new CNV from growing by blocking the effects of a growth factor these blood vessels need to thrive. Anti-VEGF medications are injected directly into your eye. Some anti-VEGF agents that have been approved for use or are currently being investigated for treating macular degeneration include:
Macugen
Pegaptanib (Macugen) is approved for the treatment of wet macular degeneration. This drug is given as a series of injections into the vitreous fluid in the eye. It helps to prevent further vision loss by stopping the formation of new blood vessels and decreasing leakage from existing blood vessels.
Lucentis
Like Macugen, ranibizumab (Lucentis) is an anti-VEGF drug used to treat wet macular degeneration. It also impedes new growth of abnormal blood vessels and helps dry up leaking vessels. However, ranibizumab may be able to reverse some of the effects of macular degeneration, not just prevent further vision loss.
Bevacizumab (Avastin)
Some doctors are prescribing this drug, which is closely related to ranibizumab, hoping that it will have effects. Bevacizumab hasn’t been approved by the Food and Drug Administration (FDA) as a treatment for macular degeneration, but it has been approved as a treatment for colon and rectal cancer. That means that the use of this medication to treat macular degeneration is currently considered an off-label use of the drug. Still, some physicians are using bevacizumab injections to treat wet macular degeneration.
Other emerging treatments, ongoing studies
Therapies under study include:
Kenalog
Triamcinolone (Kenalog) is a steroid drug used to treat eye inflammation and swelling (edema). Clinical trials are under way to determine whether Kenalog injections, alone or in combination with other therapies, might improve vision in people with macular degeneration. Some ophthalmologists are using Kenalog injections in combination with photodynamic therapy, hoping to maximize the therapeutic effect of photodynamic therapy.
Rheophoresis
In this procedure, blood is removed from your body, filtered and then returned to your body. The idea behind this therapy is that rheopheresis may remove substances from your blood that contribute to poor blood flow in the blood vessels nourishing your retina.
There are other ongoing studies investigating the use of implantable optical devices.
Because research into new treatments for macular degeneration is ongoing, it is a good idea to visit your doctor periodically to see if a new treatment might be available.
Diet
Nothing you do can change your race or genetic makeup or keep you from getting older — major risk factors for macular degeneration. However, the following measures may help prevent or delay the progression of macular degeneration:
Eat foods containing antioxidants – A nutritionally balanced diet with plenty of leafy greens, fruits and other vegetables may be among the most important factors in promoting good retinal health. People at high risk of the advanced stages of macular degeneration may be able to lower that risk with a dietary supplement of antioxidants, zinc, and copper. Antioxidants are substances that prevent oxidative damage to tissue, such as the retina.
Foods with antioxidants are those rich in vitamins A, C and E – It helps to eat a nutritionally balanced, low-fat diet containing five or more servings of fruits and vegetables every day. People who eat diets rich in vegetables, particularly leafy green vegetables may have a lower risk of macular degeneration.
High levels of the antioxidants lutein and zeaxanthin in your blood may help protect your retina, although there are no conclusive studies demonstrating that supplements of these nutrients can slow vision loss. Lutein and zeaxanthin are nutrients found in high concentrations in egg yolks, corn and spinach. The National Eye Institute is currently sponsoring a clinical trial to assess the efficacy of lutein and zeaxanthin in lowering the risk of macular degeneration.
Take supplements
Research called the Age-Related Eye Disease Study (AREDS) showed that a daily supplement of 500 milligrams (mg) of vitamin C, 400 international units (IU) of vitamin E, 15 mg of beta carotene (often as vitamin A — up to 25,000 IU), 80 mg of zinc (as zinc oxide) and 2 mg of copper (as cupric oxide) reduced the risk of progressing to moderate or severe vision loss by up to 25 percent. For people with moderate to advanced macular degeneration, the findings from AREDS indicate that taking high doses of zinc, beta carotene, and vitamins C and E is effective in reducing the risk of further vision loss.
Eat fish
Regular consumption of fish and the omega-3 fatty acids found in fish can result in a reduced risk of macular degeneration, according to the findings of a study published in July 2006. Use discretion if you’re considering more frequent consumption of fish; certain types of fish may contain high levels of toxins and other contaminants.
Sunglasses
Wear sunglasses that block out the harmful ultraviolet light – Orange-, yellow- or amber-tinted lenses can filter out both ultraviolet light and blue light. The main purpose of these glasses is to protect the surface of your eye and the skin of your eyelids. Because ultraviolet light has also been associated with the development of cataracts, the use of sunglasses may help reduce the risk of cataracts as well. Look for glasses that filter 99 percent to 100 percent of ultraviolet A (UVA) and ultraviolet B (UVB) rays. UVA penetrates deeper, while UVB has a more superficial effect.
Manage your other diseases
If you have cardiovascular disease or high blood pressure, take your medication and follow your doctor’s instructions for controlling the condition.
Get regular eye exams
Early detection of macular degeneration increases your chances of preventing serious vision loss. If you are older than 40, get an exam every two to four years and if you are older than 65 get an exam every year or two. If you have a family history of macular degeneration, have your eyes examined more frequently, perhaps annually.
Screen your vision regularly
If you have received a diagnosis of early-stage macular degeneration, your doctor may suggest that you regularly monitor your vision at home with an Amsler grid. Doing so may help you to detect subtle changes in your vision at the earliest possible time and seek help promptly.
If you have some vision loss because of macular degeneration, your eye doctor can prescribe optical devices called low-vision aids that will help you see better for close-up work. Or your doctor may refer you to a low-vision specialist. In addition, a wide variety of support services and rehabilitation programs are available that may help you adjust your lifestyle.
Lifestyle:
- Use caution when driving.
- Seek help traveling – Use public transportation or ask family members to help, especially with night driving.
- Travel with others – Contact your local area agency on aging for a list of vans and shuttles, volunteer driving networks or ride shares.
- Get good glasses
- Use magnifiers
- View with large type on the Internet
- Obtain specialized appliances – Some clocks, radios, telephones and other appliances have extra-large numbers.
- Have proper light in your home – This will help with reading and other activities.
- Remove hazardous things in the home – Eliminate throw rugs and other possible tripping hazards in your home.
- Ask friends and family members for help
- Socialize with friends – Do not stay in the house all day.
- Use the Internet – The Internet is a good source for support groups and resources for people with macular degeneration.
- Talk to your doctor – Ask your doctor about receiving professional help to make your home safer and more convenient for you to use.