Ways to Address Your Root Causes of Infertility Naturally
Table of Contents
- Symptoms
- Causes
- Causes of male infertility
- Impaired shape and movement of sperm
- Absent sperm production in testicles
- Low sperm concentration
- Varicocele
- Undescended testicle (cryptorchidism)
- Testosterone deficiency (male hypogonadism)
- Klinefelter’s syndrome
- Infections
- Sexual issues
- Retrograde ejaculation
- Blockage of the epididymis or ejaculatory ducts
- No semen (ejaculate)
- Misplaced urinary opening (hypospadias)
- Anti-sperm antibodies
- Cystic fibrosis
- Environmental Causes include:
- Specific causes include:
- Causes of female infertility
- Infertility in endometriosis also may be due to:
- Diagnosis
- Tests for men
- Tests for women
- Treatment
- Clomiphene citrate (Clomid, Serophene)
- Human menopausal gonadotropin, or hMG (Repronex, Pergonal)
- Follicle-stimulating hormone, or FSH (Gonal-F, Follistim, Bravelle)
- Human chorionic gonadotropin, or hCG (Ovidrel, Pregnyl)
- Gonadotropin-releasing hormone (Gn-RH) analogs
- Letrozole (Femara)
- Metformin (Glucophage)
- Bromocriptine
- Surgery
Symptoms
Causes
Causes of male infertility
Impaired shape and movement of sperm
Sperm must be properly shaped and able to move rapidly and accurately toward the egg for fertilization to occur. If the shape and structure (morphology) of the sperm are abnormal or the movement (motility) is impaired, sperm may not be able to reach the egg.
Absent sperm production in testicles
Complete failure of the testicles to produce sperm is rare, affecting very few infertile men.
Low sperm concentration
A normal sperm concentration is greater than or equal to 20 million sperm per milliliter of semen. A count of 10 million or fewer sperm per milliliter of semen indicates low sperm concentration (subfertility). A count of 40 million sperm or higher per milliliter of semen indicates increased fertility.
Varicocele
A varicocele is a varicose vein in the scrotum that may prevent normal cooling of the testicle and raise testicular temperature, preventing sperm from surviving.
Undescended testicle (cryptorchidism)
This occurs when one or both testicles fail to descend from the abdomen into the scrotum during fetal development. Undescended testicles can cause mild to severely impaired sperm production. Because the testicles are exposed to the higher internal body temperature compared to the temperature in the scrotum, sperm production may be affected.
Testosterone deficiency (male hypogonadism)
Infertility can result from disorders of the testicles themselves, or an abnormality affecting the hypothalamus or pituitary glands in the brain that produce the hormones that control the testicles.
Klinefelter’s syndrome
In this disorder of the sex chromosomes, a man has two X chromosomes and one Y chromosome instead of one X and one Y. This causes abnormal development of the testicles, resulting in low or absent sperm production. Testosterone production also may be lower.
Infections
Infection may temporarily affect sperm motility. Repeated bouts of sexually transmitted diseases (STDs), such as chlamydia and gonorrhea, are most often associated with male infertility. These infections can cause scarring and block sperm passage. Mycoplasma is an organism that may fasten itself to sperm cells, making them less motile. If mumps, a viral infection usually affecting young children, occurs after puberty, inflammation of the testicles can impair sperm production. Inflammation of the prostate (prostatitis), urethra or epididymis also may alter sperm motility.
Sexual issues
Often treatable, problems with sexual intercourse or technique may affect fertility. Difficulties with an erection of the penis (erectile dysfunction), premature ejaculation, painful intercourse (dyspareunia), or psychological or relationship problems can contribute to infertility. Use of lubricants such as oils or petroleum jelly can be toxic to sperm and impair fertility.
Retrograde ejaculation
This occurs when semen enters the bladder during orgasm rather than emerging out through the penis. Various conditions can cause retrograde ejaculation including diabetes, bladder, prostate or urethral surgery, and the use of psychiatric or antihypertensive drugs.
Blockage of the epididymis or ejaculatory ducts
Some men are born with a blockage of the part of the testicle that contains sperm (epididymis) or ejaculatory ducts. And some men who seek treatment for infertility lack the tubes that carry sperm (vasa deferentia).
No semen (ejaculate)
The absence of ejaculate may occur in men with spinal cord injuries or diseases. This fluid transports sperm through the penis into the vagina.
Misplaced urinary opening (hypospadias)
A birth defect can cause the urinary (urethral) opening to be abnormally located on the underside of the penis. If not surgically corrected, this condition can prevent sperm from reaching the cervix.
Anti-sperm antibodies
Antibodies that target sperm and weaken or disable them usually occur after surgical blockage of part of the vas deferens for male sterilization (vasectomy). Presence of these antibodies may complicate the reversal of a vasectomy.
Cystic fibrosis
Men with cystic fibrosis often have missing or obstructed vasa deferentia.
Male’s health and the way he lives can affect infertility such as:
- Emotional stress
- Malnutrition. Deficiencies in nutrients such as vitamin C, selenium, zinc and folate may contribute to infertility
- Obesity
- Cancer and its treatment
- Alcohol and drugs. The use of certain drugs also can contribute to infertility
- Severe injury
- Surgery
- Diabetes
- Thyroid disease
- HIV/AIDS
- Cushing’s syndrome
- Anemia
- Heart attack
- Liver
- kidney failure
- Age
Environmental Causes include:
Environmental elements
Specific causes include:
Pesticides and other chemicals
Herbicides and insecticides may cause female hormone-like effects in the male body and may be associated with reduced sperm production. Exposure to such chemicals also may contribute to testicular cancer. Men exposed to hydrocarbons, such as ethylbenzene, benzene, toluene, xylene and aromatic solvents used in paint, varnishes, glues, metal degreasers and other products, may be at risk of infertility. Men with high exposure to lead also may be more at risk.
Testicular exposure to overheating
Frequent use of saunas or hot tubs can elevate your core body temperature. This may impair your sperm production and lower your sperm count.
Substance abuse
Cocaine or heavy marijuana use may temporarily reduce the number and quality of your sperm.
Smoking
Men who smoke may have a lower sperm count than do those who don’t smoke.
Causes of female infertility
Fallopian tube damage or blockage
This condition usually results from inflammation of the fallopian tube (salpingitis). Chlamydia is the most frequent cause. Tubal inflammation may go unnoticed or cause pain and fever.
Tubal damage with scarring is the major risk factor of a pregnancy in which the fertilized egg is unable to make its way through the fallopian tube to implant in the uterus (ectopic pregnancy). One episode of tubal infection may cause fertility difficulties. The risk of ectopic pregnancy increases with each occurrence of tubal infection.
Endometriosis
Endometriosis occurs when the tissue that makes up the lining of the uterus grows outside of the uterus. This tissue most commonly is implanted on the ovaries or the lining of the abdomen near the uterus, fallopian tubes, and ovaries. These implants respond to the hormonal cycle and grow, shed and bleed in sync with the lining of the uterus each month, which can lead to scarring and inflammation. Pelvic pain and infertility are common in women with endometriosis.
Infertility in endometriosis also may be due to:
- Ovarian cysts (endometriomas). Ovarian cysts may indicate advanced endometriosis and often are associated with reduced fertility. Endometriomas can be treated with surgery.
- Scar tissue. Endometriosis may cause rigid webs of scar tissue between the uterus, ovaries and fallopian tubes. This may prevent the transfer of the egg to the fallopian tube.
- Ovulation disorders. Some cases of female infertility are caused by ovulation disorders. Disruption in the part of the brain that regulates ovulation (hypothalamic-pituitary axis) can cause deficiencies in luteinizing hormone (LH) and follicle-stimulating hormone (FSH). Even slight irregularities in the hormone system can affect ovulation.
- Elevated prolactin (hyperprolactinemia). The hormone prolactin stimulates breast milk production. High levels in women who aren’t pregnant or nursing may affect ovulation. An elevation in prolactin levels may also indicate the presence of a pituitary tumor. In addition, some drugs can elevate levels of prolactin. Milk flow not related to pregnancy or nursing (galactorrhea) can be a sign of high prolactin.
- Polycystic ovary syndrome (PCOS). In PCOS, increased androgen production prevents the follicles of the ovaries from producing a mature egg. Small follicles that start to grow but can’t mature to ovulation remain within the ovary. A persistent lack of ovulation may lead to mild enlargement of the ovaries. Without ovulation, the hormone progesterone isn’t produced and estrogen levels remain constant. Elevated levels of androgen may cause increased dark or thick hair on the chin, upper lip or lower abdomen as well as acne and oily skin.
- Early menopause (premature ovarian failure). Early menopause is the absence of menstruation and the early depletion of ovarian follicles before age 35.
- Benign uterine fibroids. Fibroids are benign tumors in the wall of the uterus and are common in women in their 30s. Occasionally they may cause infertility by interfering with the contour of the uterine cavity, blocking the fallopian tubes.
- Pelvic adhesions. Pelvic adhesions are bands of scar tissue that bind organs after pelvic infection, appendicitis, or abdominal or pelvic surgery. They may limit the functioning of the ovaries and fallopian tubes and impair fertility. Scar tissue formation inside the uterine cavity after a surgical procedure may result in a closed uterus and ceased menstruation (Asherman’s syndrome). This is most common following surgery to control uterine bleeding after giving birth.
- Medications. Temporary infertility may occur with the use of certain medications. In most cases, fertility is restored when the medication is stopped.
- Thyroid problems. Disorders of the thyroid gland, either too much thyroid hormone (hyperthyroidism) or too little (hypothyroidism), can interrupt the menstrual cycle and cause infertility.
- Cancer and its treatment. Certain cancers — particularly female reproductive cancers — often severely impair female fertility. Both radiation and chemotherapy may affect a woman’s ability to reproduce. Chemotherapy may impair reproductive function and fertility more severely in men than in women.
- Cushing’s disease
- Sickle cell disease
- HIV/AIDS
- Kidney disease
- Diabetes
Diagnosis
If you and your partner are unable to achieve conception within a reasonable time and would like to do so, seek help. The woman’s gynecologist, the man’s urologist or your family doctor can determine whether there’s a problem that requires a specialist or clinic that treats infertility problems.
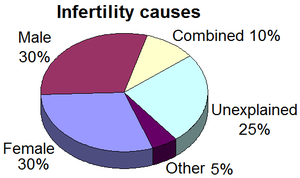
Some infertile couples have more than one cause of their infertility. Thus, your doctor will usually begin a comprehensive infertility examination of both you and your partner.
Before undergoing infertility testing, be aware that a certain amount of commitment is required. Your doctor or clinic will need to determine what your sexual habits are and may make recommendations about how you may need to change those habits. The tests and periods of trial and error may extend over several months.
Evaluation is expensive and in some cases involves operations and uncomfortable procedures, and the expenses may not be reimbursed by many medical plans. Finally, there’s no guarantee, even after all testing and counseling, that conception will occur. However, for couples who are eager to have their own child, such an evaluation is best. It may result in a successful pregnancy.
Tests for men
General physical examination. This includes an examination of your genitals and questions concerning your medical history, illnesses and disabilities, medications and sexual habits. Semen analysis. Your doctor may ask for a specimen of ejaculated semen.
This is generally obtained by masturbating or by interrupting intercourse and ejaculating your semen into a clean container. Your doctor will provide instructions. Such a specimen may be required more than once. A laboratory analyzes your semen specimen for quantity, color, and presence of infections or blood. Detailed analysis of the sperm also is done. The laboratory will determine the number of sperm present and any abnormalities in the shape and movement (motility) of the sperm. Often sperm counts fluctuate from one specimen to the next. Hormone testing. A blood test to determine the level of testosterone and other male hormones is common.
Tests for women
Confirmation of ovulation
Hysterosalpingography
Laparoscopy
Urinary luteinizing hormone (LH) detector kits
Ovarian reserve testing
Unexplained infertility
Treatment
Fertility drugs (ovulation induction) include:
Clomiphene citrate (Clomid, Serophene)
Human menopausal gonadotropin, or hMG (Repronex, Pergonal)
Follicle-stimulating hormone, or FSH (Gonal-F, Follistim, Bravelle)
Human chorionic gonadotropin, or hCG (Ovidrel, Pregnyl)
Gonadotropin-releasing hormone (Gn-RH) analogs
Letrozole (Femara)
Metformin (Glucophage)
Bromocriptine
Surgery
In vitro fertilization (IVF)
This is the most effective ART technique. IVF involves retrieving mature eggs from a woman, fertilizing them with a man’s sperm in a dish in a laboratory and implanting the embryos in the uterus three to five days after fertilization. IVF often is recommended as first-line therapy and is the treatment of choice if both fallopian tubes are blocked. It’s also widely used for a number of other conditions, such as endometriosis, unexplained infertility, cervical factor infertility, male factor infertility, and ovulation disorders.
Electroejaculation
Electric stimulus brings about ejaculation to obtain semen. This procedure can be used in men with a spinal cord injury who can’t otherwise achieve ejaculation.
Surgical sperm aspiration
This technique involves removing sperm from part of the male reproductive tract such as the epididymis, vas deferens or testicle. This allows retrieval of sperm if a blockage is present.
Intracytoplasmic sperm injection (ICSI)
This technique consists of a microscopic technique (micromanipulation) in which a single sperm is injected directly into an egg to achieve fertilization in conjunction with the standard IVF procedure. ICSI has been especially helpful in couples who have previously failed to achieve conception with standard techniques. For men with low sperm concentrations, ICSI dramatically improves the likelihood of fertilization.
Assisted Hatching
This technique attempts to assist the implantation of the embryo into the lining of the uterus.
ART
ART works best when the woman has a healthy uterus, responds well to fertility drugs, and ovulates naturally or uses donor eggs. The man should have healthy sperm, or donor sperm should be available. The success rate of ART gradually diminishes after age 32.
Certain complications exist with the treatment of infertility. These include:
Multiple pregnancies
Although the most common complication of ART is multiple pregnancies, ART isn’t the direct cause of a number of the extreme cases of septuplets or octuplets reported in the media. The number of quality embryos kept and matured to fetuses and birth ultimately is a decision made by the couple. If too many babies are conceived, the removal of one or more fetuses (multifetal pregnancy reduction) is possible to improve survival odds for the other fetuses.
Ovarian hyperstimulation syndrome (OHSS)
If overstimulated, a woman’s ovaries may enlarge and cause pain and bloating. Mild to moderate symptoms often resolve without treatment, although pregnancy may delay recovery. Rarely, fluid accumulates in the abdominal cavity and chest, causing abdominal swelling and shortness of breath. This accumulation of fluid can deplete blood volume and lower blood pressure. Severe cases require emergency treatment. Younger women and those who have polycystic ovary syndrome have a higher risk of developing OHSS than do other women.
Bleeding or infection
As with any invasive procedure, there is a risk of bleeding or infection.
Low birth weight
The greatest risk for low birth weight is multiple pregnancies. In single live births, there may be a greater chance of low birth weight associated with ART.
Birth defects
Significant concern exists regarding the possible relationship between ART and birth defects. More research is necessary to confirm these findings. Weigh this factor if you’re considering whether to take advantage of this treatment. ART is the most successful fertility-enhancing therapy to date.